A CASE OF 65 YEARS OLD FEMALE WITH ACUTE INTERSTITIAL PANCREATITIS
This is an E logbook to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here, we discuss our individual patient's problems through series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence-based inputs. This E-logbook also reflects my patient-centered online portfolio and your valuable inputs in the comments are welcome.
I would like to thank Dr. Raveen sir (Gen Med PG) for providing me the information related to the case.
This is a case of 65 years old female who came to the hospital on 10th June with :
CHIEF COMPLAINTS:
1) Pain abdomen since 2 days
2) Abdominal distension since 9th evening
3) Nausea since 9th evening
HISTORY OF PRESENT ILLNESS :
The patient was apparently asymptomatic 2 days back then she started experiencing pain abdomen which was diffuse, sudden in onset, colicky type, non-radiating with no aggravating and relieving factors.
Then the patient developed abdominal distension in the evening, which was sudden in onset and accompanied by nausea.
The patient passed stools 2 days back, did not pass flatus. She also has a H/O hard stools and irregular bowel habits.
No H/O white discharge P/V
No H/O bleeding P/R
The patient tested COVID-19 positive (RTPCR positive) on 10th June.
PAST HISTORY:
No H/O similar complaints in the past.
Not a K/C/O Diabetes Mellitus, hypertension, asthma, CKD,CHD, TB, epilepsy.
PERSONAL HISTORY :
Diet: Mixed
Appetite: Normal
Sleep: adequate
Bowel habits : Irregular bowel habits
Bladder movements: Regular
Addictions: consumes toddy occasionally
No known allergies
FAMILY HISTORY : Insignificant
GENERAL EXAMINATION:
The patient was examined in a well lit room with informed consent.
Patient was conscious, coherent and cooperative, well oriented to time, place and person.
- Pallor : Absent
- Icterus: Absent
- Cyanosis: Absent
- Clubbing: Absent
- Lymphadenopathy : Absent
- Edema : Absent
VITALS :
- Temperature : Afebrile
- BP -150/80mmhg
- PR- 150/min
- RR- 20 cpm
- Spo2- 98% at RA
SYSTEMIC EXAMINATION :
CVS : S1 and S2 heard
No added thrills and murmurs
RS : Normal vesicular breath sounds heard
B/L inspiratory crepts + in ISA, IAA
Position of trachea : Central
PER ABDOMEN : Abdominal distension + in the upper abdomen
- Diffuse tenderness +
- Guarding present, no rigidity
- No engorged veins
- Spleen - normal
P/R Examination : Rectum roomy
No mass, soft stools present, glove stained with stools
CNS: NAD
LAB INVESTIGATIONS :
CBP :
- Hb- 14.1
- TLC - 16,400
- Neutrophils : 90
- Lymphocytes : 5
- Eosinophils : 3
- Monocytes : 2
- Basophils : 0
- Platelet count : 3.56
- Normocytic normochromic with neutrophilic leucocytosis
RENAL FUNCTION TESTS :
- Urea : 44
- Creatinine : 1.1
- Uric acid : 3.4
- Ca+ : 10.0
- Phosphorus : 2.6
- Na+ : 134
- K+ : 3.2
- Cl- : 98
LIVER FUNCTION TESTS :
- TB : 0.96
- DB : 0.17
- SGPT(ALT): 39
- SGOT (AST): 42
- Alk Phosphate : 247
- TP: 5.3
- Albumin : 3.1
- A/G ratio: 1.44
Sr. AMYLASE : 980
Sr. LIPASE : 191
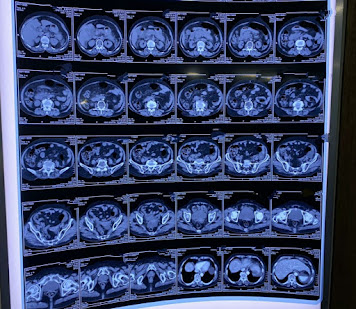
CE CT SCAN ABDOMEN :
ECG :
DIAGNOSIS : Acute interstitial pancreatitis with ? Covid-19 pneumonia ( RTPCR positive)
TREATMENT:
- NBM until further orders
- IVF 20 NS, 20RL, 10 DNS @ 150ml/hr
- INJ.PANTOP 40 mg OD
- INJ.TRAMADOL 1 Amp IV in 100ml NS IV BD
- B.P CHARTING 8th HOURLY







Comments
Post a Comment