Case of a 55 year old male with fever and altered sensorium
This is an E logbook to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here, we discuss our individual patient's problems through series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence-based inputs. This E-logbook also reflects my patient-centered online portfolio and your valuable inputs in the comments are welcome.
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
CASE PRESENTATION :
This is a case of a 55 year old male, farmer by occupation who presented with:
CHIEF COMPLAINTS:
Fever since 4 days
Altered sensorium since 1 day
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 4 days back, then he developed high grade fever with chills, with no diurnal variation.
H/o altered sensorium since 1 day.
Patient had apparently stopped taking OHA for 3 days.
He was talking irrelevantly and was unable to recognize his relatives since 6/2/22 morning.
So he was taken to Nalgonda hospital where his TLC:13,000, creatinine: 2.9 . He was shifted to the present hospital for further management
He was able to move all his four limbs.
No H/O vomitings, headache, seizures.
PAST HISTORY :
Patient had H/O TB 2 years back for which he used ATT for 6 months.
He was a K/C/O Type 2 Diabetes mellitus since 1 year and from then he has been on OHA.
No H/O HTN, asthma, CHD.
PERSONAL HISTORY :
Diet: Mixed
Appetite: Normal
Sleep: Adequate
Bowel and bladder habits: Regular
Addictions: H/O smoking since 30yrs (1 pack per day)
Consumption of alcohol about 180ml/day since 30 years, decreased intake since 2 years after diagnosis of TB.
FAMILY HISTORY: Insignificant
GENERAL EXAMINATION:
Patient is conscious, incoherent, non-cooperative
No pallor, icterus, clubbing, cyanosis, lymphadenopathy, edema
VITALS :
Temperature: 97°F
Pulse rate :126 bpm
Blood Pressure : 190/80 mmHg
Respiratory rate : 28cpm
SPO2 - 97 % at RA
GRBS- 436 mg/dl
SYSTEMIC EXAMINATION:
CVS : S1 S2 heard , no murmurs
RS: Bilateral Air entry present, NVBS
Dyspnoea present
P/A : soft,non tender
CNS:
Patient is conscious, not oriented ,non cooperative
HMF: couldn't be elicited.
Motor system: unable to move right LL against gravity.
Tone - Rt Lt
U/L N N
L/L ?HYPO N
Reflexes:
Biceps, triceps, supinator, knee, ankle: can't be elicited.
O/E Neck stiffness present , appears to be? Spondyloarthropathy
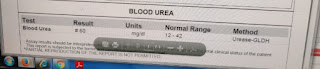
LAB INVESTIGATIONS:
On 6/2/22
On 7/2/ 22
On 8/2/22:
ECG:
CXR:
PROVISIONAL DIAGNOSIS:
Hyperosmolar Nonketotic state ē Diabetic Nephropathy
TREATMENT :
1.IVF 2 UNITS NS IV_BOLUS/STAT.
AND THEN IVF NS@100ML/HR
2.INJ.HAI 6U/IV/STAT
3.INJ.HUMAN ACTRAPID 1ML(40U)
4.INJ.THIAMINE 1AMP IN 100ML NS/IV/OD
5.INJ.OPTINEURON 1 AMP IN 100ML NS/IV/OD
6.GRBS MONITORING-EVERY HOURLY.
7.INJ.MONOCEF 2GM/IV/BD.
























Comments
Post a Comment