2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A. Pharmacological interventions used for the patient :
i) INJ.AUGMENTIN - amoxicillin + clavulanic acid
MOA : Amoxicillin binds to penicillin-binding proteins within the bacterial cell wall and inhibits bacterial cell wall synthesis. Clavulanic acid is a β-lactam, structurally related to penicillin, that may inactivate certain β-lactamase enzymes.
Indication: To treat bacterial infections, shorten the course of the disease, prevent further deterioration of lung function, and prolong the period between exacerbations.
ii) TAB.AZITHROMYCIN
MOA: Azithromycin prevents bacteria from growing by interfering with their protein synthesis. It binds to the 50S subunit of the bacterial ribosome, thus inhibiting translation of mRNA.
Indication : To treat Acute exacerbations of COPD
iii) INJ.LASIX - Furosemide
MOA: Furosemide, like other loop diuretics, acts by inhibiting the luminal Na-K-Cl co-transporter in the thick ascending limb of the loop of Henle, by binding to the chloride transport channel, thus causing sodium, chloride, and potassium loss in urine.
Indication : To treat pedal edema
iv) TAB PANTOP
MOA : In the gastric parietal cell of the stomach, pantoprazole covalently binds to the H+/K+ ATP pump to inhibit gastric acid and basal acid secretion. The covalent binding prevents acid secretion for up to 24 hours and longer.
Indication : To treat the acidity caused by antibiotics
v) INJ.HYDROCORTISONE :
MOA : Hydrocortisone is as a Corticosteroid Hormone Receptor Agonist. It works by reducing inflammation (irritation and swelling) in the body.
vi) NEB. with IPRAVENT, BUDECORT
MOA :Ipratropium is an acetylcholine antagonist via blockade of muscarinic cholinergic receptors. Blocking cholinergic receptors decreases the production of cyclic guanosine monophosphate (cGMP). This decrease in the lung airways will lead to decreased contraction of the smooth muscles.
- Budesonide is a potent topical anti-inflammatory agent. [19] It binds and activates glucocorticoid receptors (GR) in the effector cell (e.g., bronchial) cytoplasm that allows the translocation of this budesonide-GR complex in the bronchi nucleus, which binds to both HDCA2 and CBP (HAT)
Indication : To treat shortness of breath
vii) TAB PULMOCLEAR
MOA : Acebrophylline is a compound which has been found to act both as a mucoregulating and a bronchodilating drug, works by relaxing the airways.
Indication :Treatment of COPD
Non-pharmacological interventions :
i) Head end elevation : The elevation of the head of bed (HOB) to a semi-recumbent position is associated with a decreased incidence of aspiration and ventilator-associated pneumonia (VAP). It also can increase the possibility of more homogeneous alveolar ventilation and possibly reduce the risk of lung injury caused by mechanical ventilation
ii) BiPAP: BiPAP therapy targets dysfunctional breathing patterns. By having a custom air pressure for when you inhale and a second custom air pressure when you exhale, the machine is able to provide relief to your overworked lungs and chest wall muscles.
Indication : To treat COPD
iii) Chest physiotherapy : Chest physiotherapy involves a number of physical techniques to help remove excess mucus from respiratory passages and improve breathing. The goal is to help patients breathe more freely and get more oxygen through the blood stream into all parts of the body.
3) What could be the causes for her current acute exacerbation?
A. The cause for her acute exacerbation could be due to infection of bronchial tree i. e Bronchiectasis which has recently developed in this patient or usage of ATT inspite of being AFB negative .
4. Could the ATT have affected her symptoms? If so how?
A. Yes, the use of ATT could have resulted in generalized weakness and SOB in the patient.
5.What could be the causes for her electrolyte imbalance?
A. Hyponatremia in this patient has occurred due to COPD as a manifestation of secondary water retention due to right heart failure.
2) NEUROLOGY:
A) Link to patient details:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A. Evolution of symptomatology:
- Alcoholic since 12 years.
- 2 years ago - Diagnosed with DM-2 and is using medication irregularly.
- 1 year ago - Seizure episode.
- 4 months ago - Seizure episode.
- 9 days ago - Irrelevant talking, laughing, short term memory loss and decreased appetite
Anatomical location of the problem: GABA receptors in the brain, lowers parts of brain mainly hypothalamus and thalamus
Primary etiology :Alcohol
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A. Pharmacological interventions :
i) IVF NS and RL :
IV fluids help maintain a patient's hydration and electrolyte levels.
ii) INJ.THIAMINE :
Thiamine replacement is treatment for Wernicke's Encephalopathy ( occurs due to thiamine deficiency ) in order to reverse mental status changes and prevent further disease progression. Parenteral thiamine is used since intestinal absorption of thiamine is impaired in the case of alcoholics.
iii) INJ.LORAZEPAM:
MOA :Lorazepam binds to benzodiazepine receptors on the postsynaptic GABA-A ligand-gated chloride channel neuron at several sites within the central nervous system (CNS). It enhances the inhibitory effects of GABA, which increases the conductance of chloride ions into the cell.Its inhibitory action in the amygdala helps with anxiety disorders
Indication : Alcohol withdrawal delirium , Wernicke's encephalopathy
iv) TAB.PREGABALIN
MOA: The site of action of both drugs is the alpha2-delta (alpha2-delta) protein, an auxiliary subunit of voltage-gated calcium channels. Pregabalin subtly reduces the synaptic release of several neurotransmitters, apparently by binding to alpha2-delta subunits, and possibly accounting for its actions in vivo to reduce neuronal excitability and seizures.
v) INJ.KCL IN NS : to treat the symptoms of Hypokalemia.
vi) SYP.POTKLOR : Potklor oral solution contains Potassium Chloride which is used to prevent and treat the low levels of potassium in the body.
3) Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
4) What is the reason for giving thiamine in this patient?
A. Wernicke's encephalopathy is an acute neurological caused by thiamine deficiency , which primarily affects the peripheral and central nervous systems. Thiamine deficiency is characteristically associated with severe alcohol use disorder.
Thiamine, also known as Vitamin B1, is a coenzyme that is essential for intricate organic pathways and plays a central role in cerebral metabolism. Thiamine-dependent enzymes function as a connection between glycolytic and citric acid cycles. Therefore, deficiency of thiamine will lead to decreased levels of alpha-keto-glutarate, acetate, citrate, acetylcholine and accumulation of lactate and pyruvate. This deficiency can cause metabolic imbalances leading to neurologic complications including neuronal cell death.Neuronal death in the mammillary bodies and thalamus were implicated in multiple cases of Wernicke encephalopathy studied.
Thus thiamine is prescribed in this patient in order to reverse the mental status changes caused by Wernicke's Encephalopathy. Parenteral thiamine is used since intestinal absorption of thiamine is impaired due to chronic addiction of alcoholic.
5) What is the probable reason for kidney injury in this patient?
A. Alcohol and diabetes could have resulted for kidney injury in the patient. Alcohol causes changes in the function of the kidneys and makes them less able to filter the blood. Alcohol also affects the ability to regulate fluid and electrolytes in the body. When alcohol dehydrates (dries out) the body, the drying effect can affect the normal function of cells and organs, including the kidneys.
6). What is the probable cause for the normocytic anemia?
A. Normocytic anemia could have occurred probably because of alcohol abuse which eventually causes iron deficiency by causing defect in cell production. Other causes could be decreased bone marrow production of RBCs, due to erythropoitin deficiency due to kidney failure. Foot ulcer resulted in blood loss which could have resulted in normocytic anemia.
7) Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why?
A. Yes., chronic alcoholism could have aggravated foot ulcer formation in this patient. Alcoholism impairs wound healing process resulting in persistent foot ulcer.
B) Link to patient details:
Questions-
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A. Evolution of symptomatology :
- Alcoholic since 30 years.
- 7 days ago - Episode of giddiness and vomiting.
- 4 days ago - Episode of giddiness, vomiting, aural fullness, Bilateral hearing loss and tinnitus and postural instability.
Anatomical location of the problem : Cerebral blood vessels
Primary etiology : Denovo hypertension, alcohol consumption, smoking
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A. Pharmacological intervations :
i) TAB.VERTIN : Betahistine
MOA: Betahistine acts as a histamine analogue through 2 modes of action(1) agonist of H1 receptors and (2) antagonist of H3 receptors.
It has a direct stimulating (agonistic) effect on H1 receptors located on blood vessels in the inner ear. It appears to act on the precapillary sphincter in the stria vascularis of the inner ear, thus reducing the pressure in the endolymphatic space.
Indications : To treat hearing loss, tinnitus .
ii) INJ.ZOFER : Ondansetron
MOA: Zofer Injection works by inhibiting the action of a chemical substance known as serotonin. Serotonin is responsible for inducing nausea and vomiting. Ondansetron binds to a receptor known as 5-HT₃, thus inhibits the binding of serotonin to it and prevents vomiting and nausea
Indication : To prevent nausea and vomiting
iii) TAB.ECOSPORIN:
MOA: The antithrombotic action of aspirin (acetylsalicylic acid) is due to inhibition of platelet function by acetylation of the platelet cyclooxygenase (COX) at the functionally important amino acid serine529.
Indication: Ischemic stroke
iv) TAB.ATORVASTATIN
MOA : Atorvastatin competitively inhibits HMG-CoA reductase. By preventing the conversion of HMG-CoA to mevalonate, statin medications decrease cholesterol production in the liver. Thus it prevents the accumulation of cholesterol in wall of the arteries and prevents blockage of blood flow to the brain.
Indication : Cerebrovascular accident
v)TAB.CLOPIDOGREL
MOA:The active metabolite of clopidogrel selectively inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequent ADP- mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation.
Indication: CVA
3) Did the patients history of de novo HTN contribute to his current condition?
A. Yes, hypertension did contribute to cerebro-vascular accident (stroke) in this patient. Blood vessels damaged by high blood pressure can narrow, rupture or leak. High blood pressure can also cause blood clots to form in the arteries leading to your brain, blocking blood flow and potentially causing a stroke.
4) Does the patients history of alcoholism make him more susceptible to ischemic or hemorrhagic type of stroke?
A. Light and moderate alcohol consumption was inversely associated only with ischemic stroke, whereas heavy drinking was associated with increased risk of all stroke types with a stronger association for hemorrhagic strokes.
C) Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A. Evolution of Symptomatology:
- 10 years ago - Paralysis of Right and Left upper and lower limbs.
- 1 year ago - Right and Left paresis
- 8 months ago - B/L pedal edema since then
- 7 months ago - Blood Infection
- 6 days ago - Pain radiating along left limb, more during palpitations
- 5 days ago - Dyspnea (NYHA grade 3) during palpitations, chest pain and chest heaviness
Anatomical location of the problem : Cervical spine and muscles of upper and lower limbs
Etiology : Use of diuretics
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
A. Risk factors for her hypokalemia: female gender, use of diuretics
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
A. ECG changes in hypokalemia include :
- Flattening and inversion of T waves in mild hypokalemia
- Q-T interval prolongation
- visible U wave
- mild ST depression
D) Link to patient details:
QUESTIONS:
1. Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
A. Normally the “consciousness system”—a specialized set of cortical-subcortical structures—maintains alertness, attention and awareness. Generalized tonic-clonic and complex partial seizures converge on the same set of anatomical structures through different mechanisms to disrupt consciousness.
E) Link to patient details:
Questions: 1) What could have been the reason for this patient to develop ataxia in the past 1 year?
A. Cerebellar damage is the most common cause of Ataxia. Since the patient has a history of frequent falls, he might have injured his cerebellum during one of his falls.
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
A. The patient has minor unattended head injuries due to his frequent falls.During the course of time the minor hemorrhages if present should have been cured on their own. Since the patient is a chronic alcoholic, the process of healing would have hindered and further contributing to its growth further more into 13 mm sized hemorrhages occupying Frontal Parietal and Temporal lobes.
F) Link to patient details:
Questions
1.Does the patient's history of road traffic accident have any role in his present condition?
A. No , the history of RTA has no role in patient's current condition. Alcohol abuse and emotional stress could have led to his current scenario.
2.What are warning signs of CVA?
A. We can spot a stroke by the following warning sings :
3.What is the drug rationale in CVA?
A. 1)TAB.ECOSPORIN:
MOA: The antithrombotic action of aspirin (acetylsalicylic acid) is due to inhibition of platelet function by acetylation of the platelet cyclooxygenase (COX) at the functionally important amino acid serine529.
Indication: Ischemic stroke
2) TAB.ATORVASTATIN
MOA : Atorvastatin competitively inhibits HMG-CoA reductase. By preventing the conversion of HMG-CoA to mevalonate, statin medications decrease cholesterol production in the liver. Thus it prevents the accumulation of cholesterol in wall of the arteries and prevents blockage of blood flow to the brain.
Indication : Cerebrovascular accident
3) TAB.CLOPIDOGREL
MOA:The active metabolite of clopidogrel selectively inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequent ADP- mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation.
Indication: CVA
4. Does alcohol has any role in his attack?
A. Yes, alcohol has a contribution in his attack. Liver damage due to too much alcohol
can stop the liver from making substances that help your blood to clot. This can
increase your risk of having a stroke caused by bleeding in your brain.
5.Does his lipid profile has any role for his attack??
A. Yes, the patient had lower HDL levels which contribute to higher risk of stroke . HDL has anti-atherosclerotic and anti-inflammatory properties and is an important component in atherosclerosis. Serum HDL-cholesterol levels are inversely related to stroke risk.
There are several mechanisms by which HDL protects against atherosclerosis, including reverse cholesterol transport, antioxidant effects, anti-inflammatory effects, antithrombotic effects, and modification of endothelial function. Thus, lower HDL levels contribute to atherosclerosis which in turn blocks the blood supply to the brain and ultimately results in stroke.
G) Link to patient details:
Questions:
1)What is myelopathy hand ?
A. There is loss of power of adduction and extension of the ulnar two or three fingers and an inability to grip and release rapidly with these fingers. These changes have been termed "myelopathy hand" and appear to be due to pyramidal tract involvement.
The main clinical features are localized wasting and weakness of the extrinsic and intrinsic hand muscles, but not accompanied by either sensory loss or spastic quadriparesis.
2)What is finger escape ?
3) What is Hoffman’s reflex?
A. Hoffman’s sign or reflex is a test that doctors use to examine the reflexes of the upper extremities. This test is a quick, equipment-free way to test for the possible existence of spinal cord compression from a lesion on the spinal cord or another underlying nerve condition.
H) Link to patient details:
Possible questions:
1) What can be the cause of her condition ?
A. As per the MRI reports , cortical vein thrombosis could be the cause for her seizures.
2) What are the risk factors for cortical vein thrombosis?
A. Risk factors :
i) Inflammatory : SLE, sarcoidosis
ii) Infections: meningitis, otitis, mastoiditis
iii) Prothrombotic conditions: antithrombin deficiency, pregnancy, hormone replacement therapy
iv) Dehydration
v) Malignancy
vi) Nephrotic syndrome
vii) Drugs: Oral contraceptives
viii) Hematological: Myeloproliferative disorders, polycythemia
ix) Vasculitis: Behcets disease wegeners granulomatosis
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
A. Use of antiepileptics has resulted in a seizure free period in the patient. She had a sudden episode of GTCS due to withdrawal of the drug Sudden discontinuation of midazolam can result in status epilepticus. Withdrawal syndrome can occur if the dose tapers too rapidly. Symptoms due to the withdrawal of benzodiazepine include irritability, clonus, hypertonicity, nausea, vomiting, diarrhea, tachycardia, and hypertension. Benzodiazepine dose tapering can be done faster in a hospital setting in high-dose abusers, but must be done more slowly in the outpatient setting in therapeutic dosage users. Withdrawal seizures usually occur in patients who have been taking these medications for long periods of time or at high doses .
4) What drug was used in suspicion of cortical venous sinus thrombosis?
A. Low molecular weight heparin was given to the patient in suspicion of cortical vein thrombosis.
3) CARDIOLOGY:
A) Link to patient details:
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
- A. Heart failure with preserved ejection fraction (HFpEF) is a complex cardiovascular syndrome presenting with an ejection fraction (EF) of greater than 50%, along with different pro-inflammatory and metabolic co-morbidities. It is characterised by structural and cellular alterations, including cardiomyocyte hypertrophy, fibrosis, and inflammation, all leading to an inability of the left ventricle to relax properly.
- In contrast, Heart failure with reduced ejection fraction HFrEF, idefined by an EF of less than 40%, is characterized by substantial cardiomyocyte loss, resulting in the development of systolic dysfunction; in other words, the inability of the left ventricle to contract properly.
RISK FACTORS AND COMORBIDITIES:
CELLULAR ALTERATIONS:
2.Why haven't we done pericardiocentesis in this patient?
A. Pericardiocentesis is done when the pericardial effusion is not resolving on its own . Here the pericardial fluid which has accumulated was resolving on its own . At the time of admission it was 2.4mm and when the patient got discharged it was 1.9 mm. So we haven't done any pericardiocentesis.
3.What are the risk factors for development of heart failure in the patient?
A. Risk Factors for development of Heart failure:
- hypertension
- smoking
- DM type 2.
- Age
- Gender
- kidney disease.
4.What could be the cause for hypotension in this patient?
A. Anemia could be the cause of hypotension in the patient. One of the severe complication of anemia is tissue hypoxia which further lead to hypotension.
B) Link to patient details:
Questions:
1.What are the possible causes for heart failure in this patient?
A. Obesity, DM, HTN and alcohol consumption contribute as risk factors for heart failure in this patient.
2.what is the reason for anemia in this case?
A. Alcohol could be the reason for anemia in this patient. Alcoholics have defective Red blood cells which will be destroyed prematurely. This will lead to anemia.
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
A. Diabetes is the main reason for blebs and non healing ulcer in this patient.
4. What sequence of stages of diabetes has been noted in this patient?
A. Sequence of stages of Diabetes :
STAGE 1: Insulin resistance
STAGE 2: Prediabetes
STAGE 3: Diabetes type 2
STAGE4: Microvascular complications
C) Link to patient details:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A. Evolution of Symptomatology:
- 10yrs ago - Operation for Hernia
- Since 2-3 yrs - Facial puffiness
- 1 yr ago - SOB grade II
- 1 yr ago - Diagnosed with Hypertension.
- Since 2 days - SOB which progressed from Grade II to Grade IV.
- Since 2 days - Decreased urine output.
- Since 1 day - Anuria
Anatomical location - Atria (SA node)
Primary Etiology - Hypertension
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A. Pharmacological interventions:
. TAB. DYTOR:
MOA: Through its action in antagonizing the effect of aldosterone, spironolactone inhibits the exchange of sodium for potassium in the distal renal tubule and helps to prevent potassium loss.
2. TAB. ACITROM
MOA: Acenocoumarol inhibits the action of an enzyme Vitamin K-epoxide reductase which is required for regeneration and maintaining levels of vitamin K required for blood clotting
3. TAB.CARVIDAS
MOA: Carvedilol works by blocking the action of certain natural substances in your body, such as epinephrine, on the heart and blood vessels. This effect lowers your heart rate, blood pressure, and strain on your heart. Carvedilol belongs to a class of drugs known as alpha and beta-blockers.
4. INJ. HAI S/C
MOA: Regulates glucose metabolism
5.TAB. DIGOXIN
MOA: Digoxin has two principal mechanisms of action which are selectively employed depending on the indication:
Positive Ionotropic: It increases the force of contraction of the heart by reversibly inhibiting the activity of the myocardial Na-K ATPase pump,an enzyme that controls the movement of ions into the heart.
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
The patient has Cardiorenal Syndrome type 4
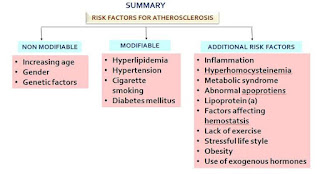
4) What are the risk factors for atherosclerosis in this patient?
A. Hypertension , physical inactivity and obesity are the risk factors for atherosclerosis in this patient
5) Why was the patient asked to get those APTT, INR tests for review?
A. Anticoagulants were prescribed to this patient. To review CVA status and predict future ischaemic strokes we asked the patient to get APTT and INR tests.
D) Link to patient details:
Questions-
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A. Evolution of symptomatology:
- Diabetes since 12 years - on medication
- Heart burn like episodes since an year- relieved without medication.
- 7 months ago- Diagnosed with pulmonary TB, completed full course of treatment, presently sputum negative.
- Hypertension since 6 months - on medication
- Shortness of breath since half an hour-SOB even at rest
Anatomical location: Coronary circulation
Etiology : - Smoking.
- High blood pressure.
- High blood cholesterol.
- Diabetes.
- Physical inactivity.
- Being overweight or obese.
- A family history of chest pain, heart disease or stroke.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A. Pharmacological interventions :
i) TAB.MET XL:
MOA: It works by relaxing the blood vessels, slowing down the heart rate. By doing this, it reduces the workload on the heart of pumping the blood effectively.
3) What are the indications and contraindications for PCI?
A. Indications:The following are the clinical indications that could require a percutaneous coronary intervention.
- Acute ST-elevation myocardial infarction (STEMI)
- Primary PCI is the recommended method of reperfusion when it can be performed in a timely fashion by experienced operators.
- STEMI and ischemic symptoms of less than 12 hours' duration.
- STEMI and ischemic symptoms of less than 12 hours' duration and contraindications to fibrinolytic therapy
- PCI improves survival in patients with significant (>50%) stenosis
- Non–ST-elevation acute coronary syndrome (NSTE-ACS)
- Early invasive therapy (within 2 hours of symptoms) recommended with refractory angina, recurrent angina, symptoms of heart failure, new or worsening mitral regurgitation, hemodynamic instability, or sustained ventricular tachycardia/fibrillation.
- A worsening of troponin levels should trigger an early therapy (within 24 hours)
- Unstable angina
- Stable angina
- Anginal equivalent (e.g., dyspnea, arrhythmia, or dizziness or syncope)
- High-risk stress test findings
- PCI is indicated for the critical coronary artery stenosis, which does not qualify for coronary artery bypass surgery (CABG)
Contraindications: Absolute Contraindications:
- Noncompliance with the procedure and inability to take dual antiplatelet therapy.
- High bleeding risk (thrombocytopenia, peptic ulcer, severe coagulopathy)
- Multiple percutaneous coronary intervention restenosis
Relative Contraindications:
- Intolerance for oral antiplatelets long-term
- Absence of cardiac surgery backup
- Hypercoagulable state
- High-grade chronic kidney disease
- Chronic total occlusion of SVG
- An artery with a diameter of <1.5 mm
- Stenosis of <50%
- Critical left main stenosis with no collateral flow or patent bypass graft
4) What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on over testing and overtreatment important to current healthcare systems?
A. PCI being performed in a patient who doesn't need it might lead to unnecessary complications and extra expenditure burden on the patient.
Research on over testing and over treatment is importance in our present health care systems because there is development of resistance in the microorganisms to the effective drugs being produced.
Over treatment might also make our body's immune system to be dependent on the medication
E) Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A. Evolution of symptomatology:
- Since 8 years - DM type 2
- 5 days ago - received COVISHIELD vaccine
- Since 3 days - Chest pain
- Since morning - Giddiness and Sweating
Anatomical location - Heart muscles
Primary etiology - Ischemia of the heart muscle.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A. I) TAB. ASPIRIN :
MOA - It inhibits COX-1 and COX-2 to decrease the Prostaglandin and thromboxane synthesis.
Indications - used as anti platelet drugs to prevent clot formation and stroke.
ii) TAB. ATORVASTATIN :
MOA - It is a HMG CoA reductase inhibitor and thus inhibits the cholesterol synthesis. It decreases VLDL, LDL in the blood, cholesterol synthesis. It increases LDL receptors in the liver and increases LDL uptake and degeneration. Thus decreasing LDL levels in the plasma.
Indications - Primary hyperlipidemias and prevention of stroke.
iii) TAB. CLOPIDOGREL :
MOA - It inhibits ADP mediated platelet aggregation by blocking P2Y12 receptor on the platelets.
Indications - To decrease risk of heart disease and prevent stroke.
iv) Inj. HAI - It is a short acting insulin.
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
A. The secondary PTCA was unnecessary in the patient as he already crossed the window period of 12 hours . In this patient it was done after 3 days of onset of symptoms which can lead to complications.
4) Gastroenterology (& Pulmonology) 10 Marks
A) Link to patient's details:
QUESTIONS:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A. Evolution of Symptomatology:
- 9 years ago : Alcoholic since then
- 5 years ago : His symptoms of pain abdomen and vomitings started and got conservative treatment.
- Stopped alcohol intake for 3 years and remained symptom free.
- 1 year ago: he again developed symptoms due to starting alcohol intake.(5-6 episodes in last year)
- From past 20 days : he drastically increased his alcohol consumption (5 bottles of toddy per day).
- 1 week ago : pain abdomen and vomiting
- 4 days ago : He developed fever, constipation and passing flatus, and has complaints of burning micturition
Anatomical location of the problem : Lung and pancreas
Primary etiology: Alcohol intake
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
A. Ulinastatin plus octreotide can significantly improve the serum and clinical parameters and reduce the incidence of complications in severe acute pancreatitis patients. And it is worthy of wider popularization.
Approach to the patient:
1) Fluid Resuscitation
2) Nutrition
3) Pain management - Opioids
4) Antibiotics
5) Endoscopy
B) Link to patient details:
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
A. Pleural effusion could be the cause for the patient's dyspnea.
Two main causes of pleural effusion are:
• Transdiaphragmatic lymphatic blockage leading to increased permeability.
• Pancreatico-pleural fistulae secondary to leak and disruption of the pancreatic duct or pseudocyst caused by an episode of acute pancreatitis.
2) Name possible reasons why the patient has developed a state of hyperglycemia.
A. The possible reason for hyperglycemia could be acute pancreatitis . Acute pancreatitis could have affected the B cells of pancreatic islets which further could have impaired Insulin production which ultimately resulted in hyperglycemia.
3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
A. Alcohol is the reason for his elevated LFT's.
Specific markers for Alcoholic Liver Disease:
•AST level is more than twice that of ALT
• Elevated levels of Gamma Glutamyl Transferase
4) What is the line of treatment in this patient
C) Link to patient details:
Possible Questions :-
1) what is the most probable diagnosis in this patient?
A. The most probable diagnosis could be ruptured liver abscess as the patient had elevated levels of alkaline Phosphatase, hyperbilirubinemia, hypoalbuminemia and hepatomegaly. .
2) What was the cause of her death?
A. Sepsis could have been the cause of her death
3) Does her NSAID abuse have something to do with her condition? How?
A. As per the patient's USG report ,she had Grade 3 RPD changes of Right kidney which suggests that she might have had an underlying CKD, which could be secondary to her NSAID abuse.(Analgesic Nephropathy)
5) Nephrology (and Urology) 10 Marks
A) Link to patient details:
1. What could be the reason for his SOB ?
A. Metabolic acidosis could be the possible reason for his SOB.The respiratory center in the brainstem is stimulated, and hyperventilation develops in an effort to compensate for the acidosis. As a result, patients may report varying degrees of dyspnea.
2. Why does he have intermittent episodes of drowsiness ?
A. The most probable cause for drowsiness in this patient could be hyponatremia which occurred due to the use of diuretics
3. Why did he complaint of fleshy mass like passage in his urine?
A. The fleshy mass like passage in his urine was due to pyuria.
4. What are the complications of TURP that he may have had?
A. Complications of TURP :
- Bladder injury.
- Bleeding.
- Blood in the urine after surgery.
- Electrolyte abnormalities.
- Infection.
- Loss of erections.
- Painful or difficult urination.
- Retrograde ejaculation (when ejaculate goes into the bladder and not out the penis)
B) Link to patient details:
Questions
1.Why is the child excessively hyperactive without much of social etiquettes ?
A. The child might be having Attention-deficit/hyperactivity disorder (ADHD) which makes him hyperactive, inattentive and impulsive. Children with ADHD are excessively hyperactive but lack an active social life. This could be the possible cause for his inactive social life.
2. Why doesn't the child have the excessive urge of urination at night time ?
A. The possible reason could be a psychomatic disorder like ADHD.
3. How would you want to manage the patient to relieve him of his symptoms?
A. Types of treatment for ADHD include
- Behavior therapy, including training for parents; and
- Medications.
Medications :
FDA has approved two types of medications—stimulants and non-stimulants—to help reduce the symptoms of ADHD. 1) Stimulants, which contain various forms of methylphenidate and amphetamine, actually have a calming effect on hyperactive children with ADHD. They are believed to increase brain levels of dopamine—a neurotransmitter associated with motivation, attention, and movement.
2) FDA has also approved three non-stimulants to treat the symptoms of ADHD: Strattera (atomoxetine), Intuniv (guanfacine), and Kapvay (clonidine). These provide a useful alternative for children who do not tolerate stimulants well.
6) Infectious Disease (HI virus, Mycobacteria, Gastroenterology, Pulmonology) 10 Marks
A) Link to patient details:
Questions:
1.Which clinical history and physical findings are characteristic of tracheo-oesophageal fistula?
A. In this patient, the following features are suggestive of TOF:
i) Cough since 2 months on taking food and liquids
Other features which favor the diagnosis of TOF are:
i) Difficulty in swallowing both solids and liquids
ii) H/O weight loss of 10 Kg since 2 months
iii) Hoarseness of voice
iv) Patient being both RVD positive and TB positive
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
A.
The most effective prevention of IRIS would involve initiation of ART before the development of advanced immunosuppression. IRIS is uncommon in individuals who initiate antiretroviral treatment with a CD4+ T-cell count greater than 100 cells/uL.
Aggressive efforts should be made to detect asymptomatic mycobacterial or cryptococcal disease prior to the initiation of ART, especially in areas endemic for these pathogens and with CD4 T-cell counts less than 100 cells/uL.
7) Infectious disease and Hepatology:
Link to patient details:
1. Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors present in it ? What could be the cause in this patient ?
A. “Alcohol can predispose to ALA through a multitude of mechanisms, including hepatic damage by alcohol, lowered body resistance and suppression of liver function due to poor nutritional status of habitual consumers of alcohol, increased presence of amoebae in the liquor prepared locally with poor regard to aseptic procedures, and depression of immune mechanisms in chronic alcoholics.”
In experimental studies, the presence of 'iron' potentiates the in-vitro growth of Entamoeba histolytica (E. histolytica), and is also known to increase its in-vivo invasiveness in animal infections. Chronic alcoholism increases the hepatic iron deposition. We hypothesized that ALA occurs more commonly in livers with a high iron load as in alcoholics.
2. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
3. Is liver abscess more common in right lobe ?
A. Liver abscess in common in right lobe as it receives more blood supply than the left lobe. Since the liver receives its blood circulation from the systemic and portal circulations, it is more susceptible to getting infections and abscesses from the bloodstream
4.What are the indications for ultrasound guided aspiration of liver abscess ?
A. Indications for ultrasound guided aspiration of liver abscess:
1) Left lobe abscess not amenable to percutaneous damage.
2) Amoebic abscess eroding into surrounding structures.
3) Liife-threatening hemorrhage with or without intraperitoneal rupture of abscess.
4) Failure of response to conservative therapy.
5) Septicemia from secondary infection.
B) Link to patient details:
QUESTIONS:
1) Cause of liver abcess in this patient ?
A. Amebic liver abscesses are caused by Entamoeba histolytica, a protozoan parasite. Amoebiasis spreads from eating food or water that has been contaminated with feces. This is sometimes due to the use of human waste as fertilizer. Amoebiasis is also spread through person-to-person contact. more in males
2) How do you approach this patient ?
3) Why do we treat here ; both amoebic and pyogenic liver abcess?
A. We treat both amoebic and pyogenic liver abscess so as to ensure complete treatment of the patient.
4) Is there a way to confirm the definitive diagnosis in this patient?
A. The diagnosis of an amebic liver abscess is made through a combination of characteristic findings on imaging and serologic testing. On imaging, there is a cystic intrahepatic cavity that is usually indistinguishable from other causes of liver abscesses. The majority of amebic liver abscesses are solitary lesions, although there can occasionally be multiple lesions, and they are more often found in the right lobe than the left. On ultrasound, the lesion is a round, well-defined hypoechoic mass . After healing, the periphery of the abscess may calcify and form a round, thin rim.
8) Infectious disease (Mucormycosis, Ophthalmology, Otorhinolaryngology, Neurology) 10 Marks
A) Link to patient details:
Questions :
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A. Evolution of symptomatology:
- 3 years ago- diagnosed with hypertension
- . 21 days ago- received vaccination at local PHC which was followed by fever associated with chills and rigors, high grade fever, no diurnal variation which was relieved on medication
- . 18 days ago- complained of similar events and went to the the local hospital, it was not subsided upon taking medication(antipyretics)
- . 11 days ago - c/o Generalized weakness and facial puffiness and periorbital oedema. Patient was in a drowsy state
- . 4 days ago-
a. patient presented to casualty in altered state with facial puffiness and periorbital oedema and weakness of right upper limb and lower limb
b. towards the evening patient periorbital oedema progressed
c. serous discharge from the left eye that was blood tinged
d. was diagnosed with diabetes mellitus
- . patient died 2 days ago
Anatomical location of the problem : Eye, nasal cavity Etiology : Diabetes
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
A. Amphotericin B has proven efficacy in the treatment of mucormycosis. At the present time, the liposomal formulation (AmBisome) is the drug of choice based on efficacy and safety data.
Experiments were performed on mice to demonstate the efficacy of Liposomal Amphotericin B and posconazole.
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?





































Comments
Post a Comment