CASE OF A 22 YEARS OLD MALE WITH COMPLAINTS OF FEVER AND PAIN DURING SWALLOWING
This is an E logbook to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here, we discuss our individual patient's problems through series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence-based inputs. This E-logbook also reflects my patient-centered online portfolio and your valuable inputs in the comments are welcome.
I would like to thank Dr.Chitra mam (Intern) for providing all the information related to the below case.
This is a case of a 22 years male , labourer by occupation who came to the casuality on 2nd June with
CHIEF COMPLAINTS :
1) High grade fever since 3 days
2) Pain during swallowing since 3 days
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 3 days back, then he developed fever which was sudden in onset, intermittent in nature not associated with chills and rigors. Fever was accompanied by pain during swallowing.
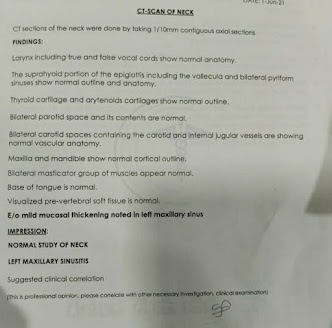
On 28th May, the patient went to local water body for fishing where he drank the water from water body. The very next day he developed a fever accompanied by pain during swallowing. He went to a local hospital where he got an USG which has E/O multiple bowel loops and CT scan of the neck which has E/O mild mucosal thickening in the left maxillary sinus. He was referred to the current hospital for further evaluation.
He also had complaints of burning micturition.
He also developed a productive cough. Patient also had a skin coloured rash on the extremities of upper limb not associated with any itching.
No H/O vomitings, loose stools , poisoning ( OP poisoning), constipation, pain abdomen.
PAST HISTORY:
Not a K/C/O DM, HTN, asthma, TB, CAD
No H/O previous surgery
FAMILY HISTORY : Insignificant
PERSONAL HISTORY :
- Diet: Mixed
- Appetite : Normal
- Bowel habits : Regular
- Micturition : Burning micturition
- No addictions
- No known allergies
Patient was examined in a well-lit room with informed consent.
Patient was conscious, coherent, cooperative and well oriented to time, place and person.
Pallor : Absent
Icterus: Absent
Cyanosis: Absent
Clubbing: Absent
Lymphadenopathy: Absent
Edema: Absent
VITALS:
2/6/21
- Temperature : 101 F
- Pulse rate : 131 bpm
- Respiratory rate : 24cpm
- B.P : 90/50 mm Hg
- SPO2 : 94% at RA
- GRBS: 70 mg/dl
3/6/21:
- Temperature : 105 F
- Pulse rate : 107 bpm
- B.P : 100/60 mm Hg

SYSTEMIC EXAMINATION :
1) CVS : S1 and S2 heard , no thrills and murmurs
2) RS: NVBS +, BAE +
Position of trachea: central
3) Per Abdomen : soft, tenderness + in epigastric region ,no guarding, no rigidity
4) CNS : NAD
Glasgow scale : 15/15
LAB INVESTIGATIONS :
CBP :
- Hb- 12.3
- TLC - 20,900
- Neutrophils : 93
- Lymphocytes : 3
- Eosinophils : 2
- Monocytes : 2
- Basophils : 0
- PCV: 34.5
- Platelet count : 1.10
- Normocytic Normochromic blood picture
- Hb- 11.9
- TLC - 22,100
- Neutrophils : 89
- Lymphocytes : 4
- Eosinophils : 2
- Monocytes : 5
- Basophils : 0
- Platelet count : 90,000 cells/cumm
- Normocytic Normochromic with neutrophillic leukocytosis and thrombocytopenia.
CUE :
- Albumin : 2+
- Pus cells : 5-6
- Epithelial cells : 3-4
- RBC : 8-10
SEROLOGY : Negative
DENGUE : Negative
RENAL FUNCTION TESTS :
- Urea : 100
- Creatinine : 1.7
- Uric acid : 7.5
- Ca+ : 9.0
- Phosphorus : 1.8
- Na+ : 136
- K+ : 4.1
- Cl- : 102
LIVER FUNCTION TESTS :
- TB : 0.70
- DB : 0.20
- ALT: 16
- AST : 107
- Alk Phosphate : 108
- TP: 5.0
- Alb: 2.7
Sr. AMYLASE : 76
Sr. LIPASE : 32













Comments
Post a Comment