Case of a 34 year old male with young onset hypertension
This is an E logbook to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here, we discuss our individual patient's problems through series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence-based inputs. This E-logbook also reflects my patient-centered online portfolio and your valuable inputs in the comments are welcome.
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
CASE PRESENTATION :
This is a case of a 34 year old male, mason by occupation came to the OPD with :
CHIEF COMPLAINTS :
- Blurring of vision in right eye > left eye since 3 years
- Slurring of speech since 1 year
Patient was apparently asymptomatic 3 years back then he developed giddiness and fell (blackouts) during his work. This episode of blackout was not associated with nausea, vomiting, vertigo,tinnitus, earfullness.Then he was taken to a local hospital and was diagnosed with high blood pressure. Since then he had been on anti-hypertensive medication.
He has slurring of speech since 1 year which was insidious in onset and gradually progressive .
Patient also complained of shortness of breath and body pains since 1 year.
Patient had a history of head trauma due to a fall in 2015 .
PAST HISTORY :
K/C/O Hypertension since 3 years (on medication)
No DM, TB, epilepsy, asthma
TREATMENT HISTORY :
On Antihypertensive medication since 3 years
Atenolol (50mg), Nicardia (10mg), Telma (40mg)
FAMILY HISTORY : Both the parents are K/C/O hypertension
PERSONAL HISTORY :
Diet : Mixed
Appetite: Normal
Sleep: Adequate
Bowel and bladder habits : Regular
Addictions:
Alcohol consumption since 15 years ( 90ml per day) stopped since 6 months
Smoking since 15 years 2 packets per day ( stopped since 6 months)
GENERAL EXAMINATION:
Patient was examined in a well lit room with informed consent
Patient was conscious, coherent and cooperative, well oriented to time, place and person.
No Pallor
No icterus
No clubbing
No Cyanosis
No Lymphadenopathy
No Edema
VITALS :
On admission :
BP: 270/140 mm hg
Patient was given Nicardia 20 mg and BP was measured after 20 mins still it was 270/140 mmHg
PR : 90bpm
RR: 18 cpm
All the peripheral pulses present
Ankle brachial index > 1.25
29/10/21:
Temperature: 98.6 F
Pulse Rate: 88 bpm
BP: Right Left
Upper limb: 130/90 140/90
Lower limb: 140 160
SpO2: 98 % @ RA
30/10/21
Temperature: 98.6 F
Pulse Rate: 60bpm
BP: Right Left
Upper limb: 170/90 170/90
Lower limb: 200 200
SYSTEMIC EXAMINATION :
CVS : S1 S2 heard, no murmurs
RS: NVBS +, no crepts
Per Abdomen: soft, non-tender
Renal bruit heard
CNS EXAMINATION :
1) HMF - INTACT
Spurring of speech present
Signs of meningeal irritation : absent
2) MOTOR SYSTEM :
Right Left
Bulk:
Inspection. N N
Palpation. N N
Tone:
UL. N. N
LL. N. N
Upper Limb:
Shoulder:
Flexion 5/5. 5/5
Extension. 5/5. 5/5
Abduction: 5/5. 5/5
Adduction: 5/5. 5/5
Elbow:
Flexion (biceps) 5/5. 5/5
Extension (triceps) 5/5. 5/5
Lower Limb:
Iliopsoas. 5/5. 5/5
Gluteus max. 5/5 5/5
Adductor femoris. 5/5 5/5
Hamstrings. 5/5 5/5
Quadriceps. 5/5 5/5
Tibialis ant. 5/5 5/5
Tibialis post. 5/5. 5/5
Ex. Digitorum L. 5/5. 5/5
Fl. Digitorum L. 4/5. 4/5
Ex. Hallucis L. 4/5. 4/5
Deep tendon reflexes:
Biceps: +2 +2
Triceps: +1 +1
Supinator: +2 +2
Knee: +3 +3
Ankle: +3 +3
Plantar: extensor flexor
Knee reflex :
Ankle reflex :
Sensory:
STT: Crude touch. + +
Pain. + +
Temp. + +
Post. Dorsal
Fine touch. present
Vibration. + +
Position. + +
Cranial nerves :
II - Blurring of vision present - Rt side > left side.
Visual acuity -
Right side - only PL/PR present.hand movements perceived . Cant count fingers.
Left side - Counting fingers 3m present.
III,IV,VI - Extra-ocular movements intact
ii) Pupil – Size - 4 mm - B/L NSRL
iii) Direct Light Reflex - Present.
V - i) Sensory - intact over the face
ii) Motor – masseter, temporalis, pterygoids
iii) Reflex
a. Corneal Reflex - present
b. Conjunctival Reflex - present
c. Jaw jerk - present.
VII - Slight deviation of mouth to left side .
IX ,X- Uvula deviated to right side .
Gag reflex intact.
XI -normal
XII - no deviation of tongue .
CEREBELLUM : Heel knee test - normal
Dysdiadochokinesia:
Finger nose couldn't be performed because of blurring of vision .
Horizontal Nystagmus present . Fast component to left side .
Couldn't perform Tandem gait .
BP- Unequal in both arms .
All peripheral pulses felt and no asymmetry noted.
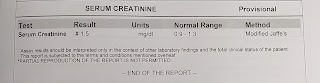
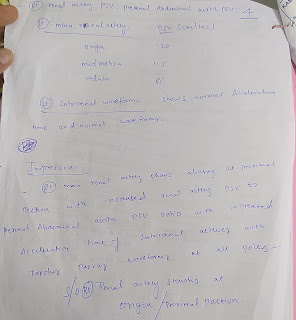
INVESTIGATIONS :
Hemogram:
CUE :

















Comments
Post a Comment